Fall Prevention After 60

In day-to-day clinic practice, the most common story is not an outdoor accident. It is an indoor slip: bathroom, kitchen, getting up at night, or missing a step. The goal of this page is to give you a practical checklist that families can actually implement.
- Why homes become high risk after 60
- Simple home changes that reduce fall risk
- Strength and balance: the strongest protective factor
- Medical causes of falls you should not ignore
- Why falls after 60 often cause fractures
- What to do immediately after a fall
- When to see an orthopaedic doctor
- Related reading
Red flags after a fall: do not wait
- Hip or groin pain, or inability to bear weight
- Wrist deformity or severe wrist pain
- Severe back pain after a simple slip (possible spine fracture)
- Head injury symptoms: vomiting, severe headache, confusion, drowsiness
- Fever, hot/swollen joint, or sudden severe swelling
Why homes become high risk after 60
Homes are designed for younger legs and faster reactions. As balance and vision change with age, small “normal” features become hazards.
- Slippery bathroom and kitchen floors (especially when wet)
- Poor lighting at night (bedroom to toilet route)
- Loose rugs, wires, cluttered walking paths
- No hand support near toilet or stairs
- Footwear that slips on tiles
Most prevention is not fancy equipment. It is small changes done consistently: lighting, rails, mats, and a strength routine.
Simple home changes that reduce fall risk
Bathroom safety

- Use anti-skid mats or textured flooring (especially near shower area)
- Install grab bars near toilet and shower
- Keep the floor dry; wipe immediately after use
- Consider a shower chair if standing balance is poor
Bedroom and living area

- Remove loose rugs or fix them firmly with anti-skid backing
- Use night lamps (bed to toilet path must be visible)
- Keep frequently used items within easy reach
- Keep the floor clear: no phone chargers or wires crossing paths
Staircase safety
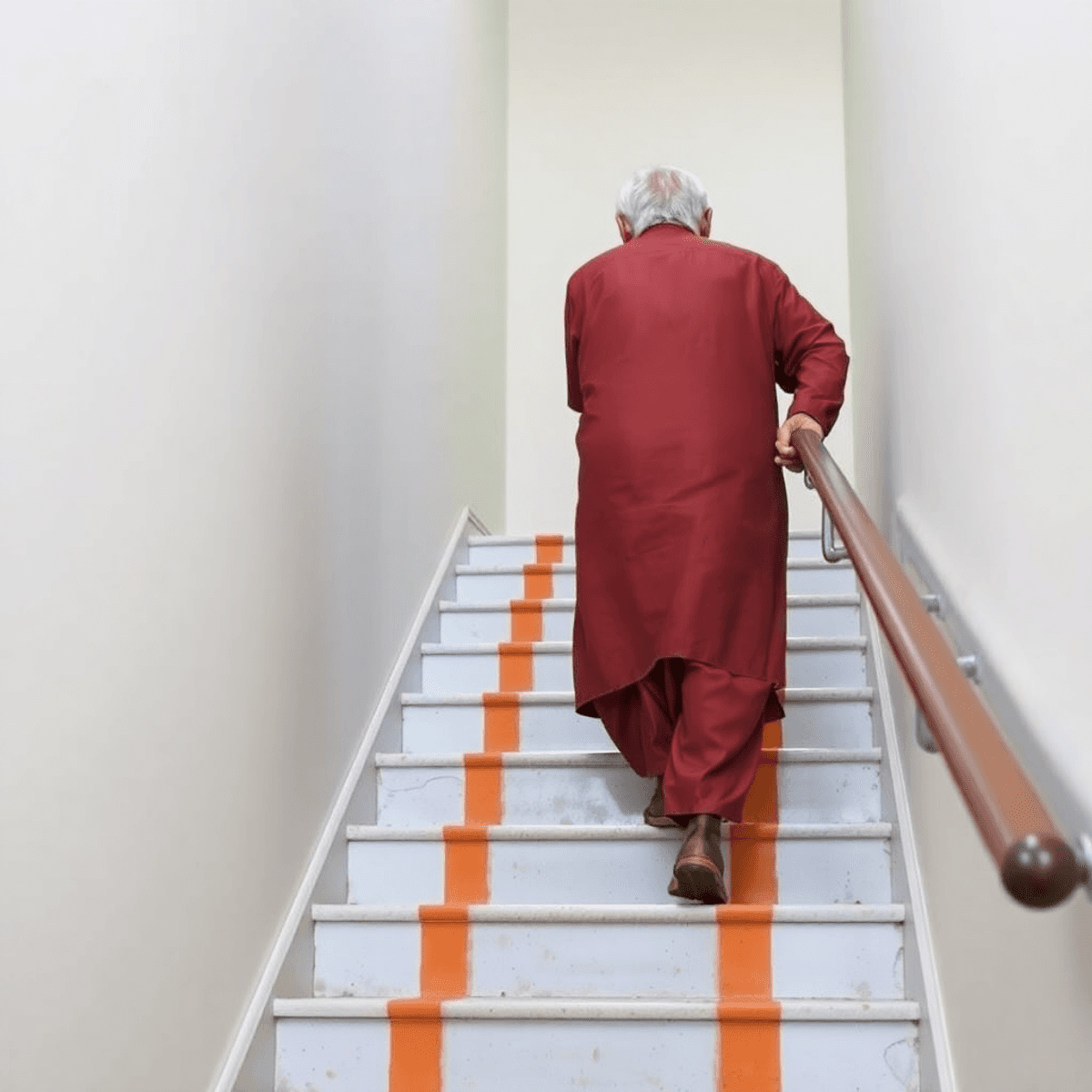
- Good lighting: no dark steps, especially at night
- Handrails on both sides if possible
- Clear step edges; avoid loose mats on steps
Fast “one-day” checklist for families
- Fix lighting: hallway + bathroom night light
- Remove loose rugs and floor clutter
- Add anti-skid mat in bathroom
- Ensure safe footwear at home (not slippery)
Strength and balance matter more than age

The single most helpful concept: capacity. If leg strength and balance capacity are low, daily tasks become risky: getting up from a chair, turning quickly, stepping into the bathroom, or climbing stairs.
- Needs support while wearing pants (single-leg balance is poor)
- Holds walls/furniture while walking at home
- Feels dizzy while getting up from bed
- Fear of falling is increasing, so walking reduces
- Sit-to-stand practice from a stable chair
- Heel raises holding a support
- Marching in place holding a support
- Tandem stance near a wall for safety
If you want supervised progression and safety checks, physiotherapy helps a lot: Physiotherapy at OrthoCure Thirumullaivoyal.
Medical causes of falls you should not ignore
Not every fall is “weakness.” Some falls are medical signals. If falls are repeated, unexplained, or associated with fainting, it needs evaluation.
- Low blood sugar episodes (diabetes medicines)
- Low blood pressure on standing (orthostatic hypotension)
- Heart rhythm problems (palpitations, blackouts)
- Stroke or mini-stroke warning signs
- Inner ear balance disorders or severe vertigo
- Medication side effects (sedatives, sleep tablets, some BP medicines)
- Vision issues (cataract, poor contrast vision at night)
Repeated unexplained falls always need medical evaluation.
If someone has two or more falls, new dizziness, or a blackout episode, treat it as a health issue—not a clumsiness issue.
If shoulder pain and stiffness became worse after a fall, frozen shoulder can be a secondary issue too: Frozen shoulder care.
Why falls after 60 often cause fractures
As bone density reduces with age (especially in osteoporosis), even a low-energy fall can cause a fracture. The pattern is often predictable.
- Hip fractures: major loss of mobility risk; often after a simple slip
- Wrist fractures: people instinctively put the hand out to break the fall
- Spine fractures: severe back pain after a small fall can be a clue
- Shoulder fractures: sideways falls commonly injure the shoulder
Do not “watch and wait” with persistent pain after a fall
Some fractures are subtle early, especially in the hip and spine. Early assessment reduces missed injuries and reduces complications.
What to do immediately after a fall
- Do not rush to stand up; sit and assess first
- Check for hip/groin pain, wrist pain, shoulder pain, back pain, head injury symptoms
- If there is severe pain, deformity, dizziness, or inability to bear weight: seek help immediately
- If pain increases over 12–24 hours, or bruising appears: get evaluated
Hip pain after a fall is a special case
If there is hip or groin pain, or the person cannot walk normally, treat it seriously and get examined with imaging when needed.
When should you see an orthopaedic doctor?
- Two or more falls in six months
- Persistent joint pain after a fall (hip, wrist, shoulder, back)
- Inability to bear weight, or walking becomes abnormal
- Known osteoporosis, or history of fragility fracture
- Recurrent near-falls (stumbling, frequent loss of balance)
Falls and fractures are closely linked to bone health. If a low-energy fall caused a fracture, it is a signal to evaluate osteoporosis risk and prevent the “next fracture.”
Want a practical fall-prevention plan for your family?
Fall prevention works best when it is simple, consistent, and realistic for your home environment. If you want a structured assessment (mobility, fracture risk, and safe next steps), we can help.
Clinic hours: Monday to Saturday 5 pm to 9 pm. Sunday 11 am to 1 pm.
No. 2, 2nd Street, Santhipuram, Thirumullaivoyal, Chennai 600062.